In California alone, about $98 billion — or 42.4% of all healthcare expenditures — is spent on chronic conditions such as arthritis, asthma, cardiovascular disease, diabetes, cancer and depression.
Those most at risk for poor healthcare outcomes include the under-served, the rapidly growing elderly population and the mentally ill. Yet pharmacists — who have the skills, training and expertise to ensure that patients receive the best treatments possible — are highly underutilized by health systems, says USC professor of clinical pharmacy Steven Chen, whose pioneering work in Los Angeles safety-net clinics has become a national model replicated at clinics across the country.
USC’s third annual Conference on Optimizing Medication Safety and Healthcare Quality: Best Practices and Collaborations for Public Health, Geriatrics and Mental Health brought together pharmacists, physicians, policy experts and healthcare leaders from across the country. Presented by USC Schaeffer Center for Health Policy & Economics and USC Mann in collaboration with Health Services Advisory Group, the conference aimed to build partnerships and share best practices for improving health outcomes while reducing total healthcare costs. Nearly 150 attended the event, held at USC on Feb. 11–12.
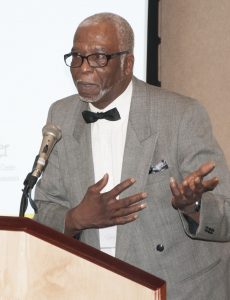
Welcoming guests from the podium was Glen L. Stimmel, interim dean of USC Mann, who launched the conference with a message promoting collaboration as the best way to serve patients in today’s changing healthcare environment, particularly in public health, geriatrics, and mental health.
Overwhelmingly, the day’s presentations focused on the changing landscape of healthcare, and opportunities for increasing value in healthcare through interdisciplinary teams, with an emphasis on the role pharmacists play in managing medication use.
Experts from across the country, including Hawaii, Montana, Arizona, North Carolina, and Maryland, shared their experiences in safety-net clinics, hospitals and community pharmacies. Attendees also looked at current approaches to helping patients manage their health, including face-to-face appointments and video telehealth consultations.
“Chronic disease management is key”
Recognizing that pharmacists can help patients improve their health while saving precious healthcare dollars, USC School of Pharmacy clinical faculty, residents, and students work in interdisciplinary teams in community settings throughout Southern California, with patients who are at a high risk for hospitalization and poor health outcomes. Thanks to a $12 million Center for Medicare and Medicaid Innovation (CMMI) grant, faculty from the USC Schaeffer Center and School of Pharmacy are able to measure the impact of comprehensive medication management on health outcomes and costs. “If you want to make an immediate impact on healthcare costs, healthcare quality and safety, chronic disease management for high-risk patients is key. It’s about collaborating with community partners, identifying patients in need, and providing comprehensive medication management,” said Chen, who shared lessons for clinical pharmacy from the initiative.
Data from the three-year program placing USC clinical pharmacy teams in AltaMed Health Services safety-net clinics shows improved medication use and health outcomes, as well as greater patient/physician satisfaction and reduced costs through a marked reduction in readmissions. “Patients loved the service,” Chen said. “If you read the letters that they submitted, (patients) identified every member of the team — the clinical pharmacy technician, the resident, the pharmacist — as being very important to their care.”
 Addressing the “triple aim” — better care, better health and smarter spending — was Dennis Wagner, MPA, Director of Quality Improvement and Innovation at the U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services, who encouraged participants to seek out opportunities for synergy, alignment and collaboration across the health care system. “When you have patients at the table, the urgency of the work accelerates,” he said. “We need to do more of what’s working. We need to accelerate the pace of that progress.”
Addressing the “triple aim” — better care, better health and smarter spending — was Dennis Wagner, MPA, Director of Quality Improvement and Innovation at the U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services, who encouraged participants to seek out opportunities for synergy, alignment and collaboration across the health care system. “When you have patients at the table, the urgency of the work accelerates,” he said. “We need to do more of what’s working. We need to accelerate the pace of that progress.”
“I see communities that are doing extraordinary work. I see clinical practices that are doing extraordinary work. I see hospitals that are doing extraordinary work. We want to replicate and improve across the system what we see in those pockets.”
With the top five leading causes of death in California being heart diseases, cancer, stroke, chronic lung disease, and Alzheimer’s disease — chronic diseases that particularly affect the 1/3rd of the state’s population that is eligible for Medicaid — partnership, collaboration and action is critical.
“If you’re going to squeeze the health system to do better, the only place that you can do that is in chronic disease,” said Jessica M. Nuñez de Ybarra, MD, MPH of the California Department of Public Health (CDPH), who shared information about California’s 10-year approach to addressing the enormous chronic disease burden, the California Wellness Plan, which she authored. “We’re not going to fix chronic disease as government, we’re going to need to do it in partnership,” she said. “We can do better, but we have to do it together.”
 Carol Peden, MD, MPH, Director of the USC Keck Center for Health System Innovation, provided a global perspective on the healthcare quality in the United States, with many lessons learned from the United Kingdom and other countries.
Carol Peden, MD, MPH, Director of the USC Keck Center for Health System Innovation, provided a global perspective on the healthcare quality in the United States, with many lessons learned from the United Kingdom and other countries.
“We have got improvement in access, cost and an amazing reduction in harm. There’s still more to do, but really good progress. Potential challenges are the holistic care of the person, both as a patient and before they become a patient, and designing our care pathways around the patient … really having the patient in the room and asking them what they want.”
“My pharmacist saved my life”
Keynote speaker Michael Metcalfe shared his personal story — one that went to the heart of the mission of the conference — as a former patient at the Center for Community Health, a safety-net clinic on Los Angeles’ Skid Row.
 “Down there, I was just a statistic,” he said. At 301 pounds and down on his luck, he would eat two pizzas for dinner and drink liters of soda. Physicians had grown frustrated with his attitude and inaction. Then one day he woke up in a hospital, after spending eight days in a diabetic coma.
“Down there, I was just a statistic,” he said. At 301 pounds and down on his luck, he would eat two pizzas for dinner and drink liters of soda. Physicians had grown frustrated with his attitude and inaction. Then one day he woke up in a hospital, after spending eight days in a diabetic coma.
It was Chen who helped him understand his condition, started him on insulin, and taught him how to be consistent with his insulin injections while learning to eat more healthfully. “Dr. Chen listened to me, he answered my questions, he gave me hope,” said Metcalfe, who began exercising, gardening and eating healthier and eventually lost more than 100 pounds. “He taught me not to live to eat, but eat to live. Now my waist is so small, I could hula hoop through a Cheerio.”
“Sometimes I get a little emotional because I credit Dr. Chen with saving my life,” says Metcalfe, who now visits the school, sharing a patient perspective with future pharmacists. “Dr. Chen taught me how to live with this disease called diabetes.”




