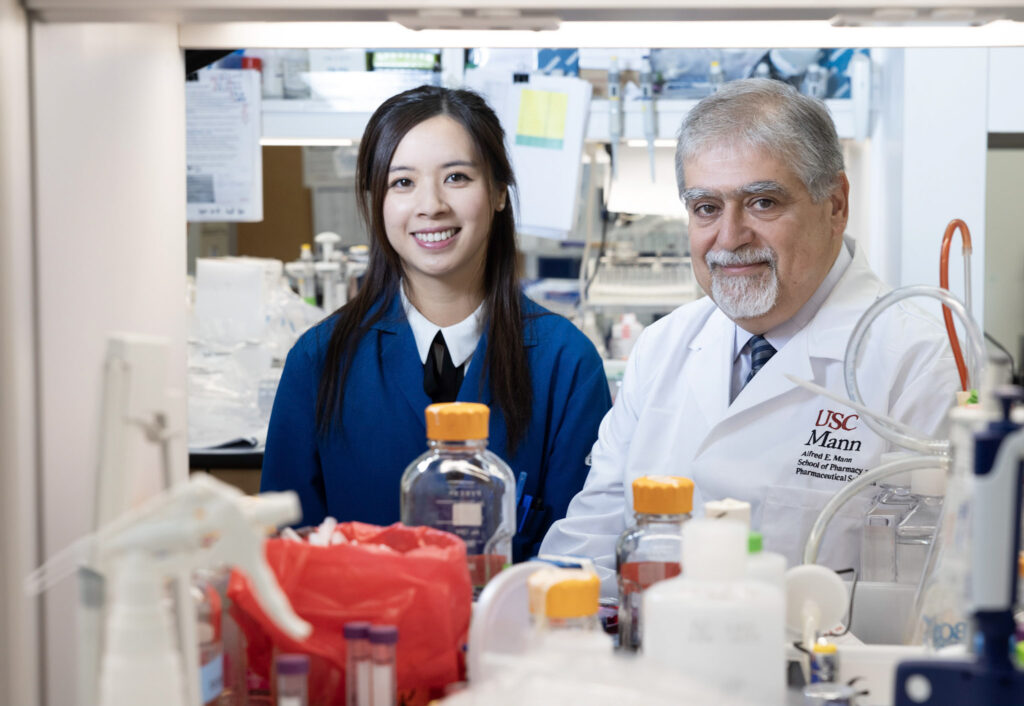
While the brain’s abilities include the capacity to answer innumerable questions, the organ itself still holds countless mysteries. Dean Vassilios Papadopoulos and postdoctoral research scholar Yiqi Christina Lin have solved one of those riddles by revealing how the brain produces pregnenolone—the “mother hormone” that is the progenitor of all neurosteroids.
Neurosteroids are formed by the brain to modulate nervous system function, and changes in their levels have been implicated in neurological conditions such as Alzheimer’s disease as well as in psychiatric and mood disorders. Therefore, neurosteroids represent a vital new frontier in biomedicine. Yet their therapeutic possibilities have barely been tapped. For example, the first approval for a neurosteroid drug did not come until 2019, when the Food and Drug Administration authorized brexanolone for postpartum depression.
“It wasn’t until the late 1980s that we learned the brain can make its own steroids,” Papadopoulos notes. “But questions remained about how this occurs because nobody had spotted the first enzyme responsible for manufacturing those steroids. We could find it in mice but not in the human brain.”
The breakthrough arose from Papadopoulos and Lin’s realization that, although cholesterol remains as the “father” of steroids, the “mother” neurosteroid pregnenolone is made by a different enzyme in the brain than in other organs. Under Papadopoulos’ direction, Lin used multiple approaches to find evidence that the enzyme metabolizing cholesterol to give birth to steroids in organs such as the gonads and adrenals hadn’t been found in the human brain because it wasn’t there.
“I spent my whole thesis proving that,” says Lin, who earned her PhD as a scientist in the Papadopoulos laboratory before continuing there as a postdoc. But then, having shown that a different enzyme must be responsible, the researchers had to determine which one that was.
Building on their previous investigations and Papadopoulos’ decades of work in steroid exploration, the scientists screened hundreds of enzymes. With the use of bioinformatics, they narrowed down their search to a handful, on which they performed drug inhibition and knockdown experiments. They ultimately identified the enzyme CYP1B1 as being involved in pregnenolone synthesis in the nervous system.
These findings, published in The Journal of Biological Chemistry in August 2023 are important since pregnenolone, as well as the neurosteroid dehydroepiandrosterone (DHEA), has been found to be elevated in Alzheimer’s patients. On the other hand, the levels of pregnenolone sulfate—a product of pregnenolone—and other neurosteroids are generally lower in patients with major depression, bipolar disorder and other mood-related conditions.
Understanding the mechanisms that drive pregnenolone production opens potential avenues to devising more effective treatments for neurological diseases and mood disorders.
The next direction to take, Lin says, “is to look at the enzyme kinetics” of CYP1B1 to form pregenolone. “Because nobody has ever studied this, we want to see the rate at which this enzyme can make these steroids.”
“It will take time,” Papadopoulos adds. “But discovering this physiological process is the link to the understanding needed to develop new treatments.”
In addition to Papadopoulos and Lin, the paper’s other authors are USC Mann PhD candidates Garett Cheung and Zeyu Zhang.
The work was supported by funds from the USC Mann School of Pharmacy and Pharmaceutical Sciences and the John Stauffer Dean’s Chair in Pharmaceutical Sciences at USC.