Among the aims of the Inflation Reduction Act (IRA) is reducing health care costs for older adults by eliminating cost sharing for certain drugs and vaccines covered by Medicare Part D. To help determine if the impact matches the IRA’s intent, a team led by Dima Qato—Hygeia Centennial Chair and Associate Professor at the USC Mann School of Pharmacy and Pharmaceutical Sciences—evaluated the impact of the IRA policy removing patient out-of-pocket costs on the uptake of shingles vaccinations, the most commonly-administered vaccine covered by Part D.
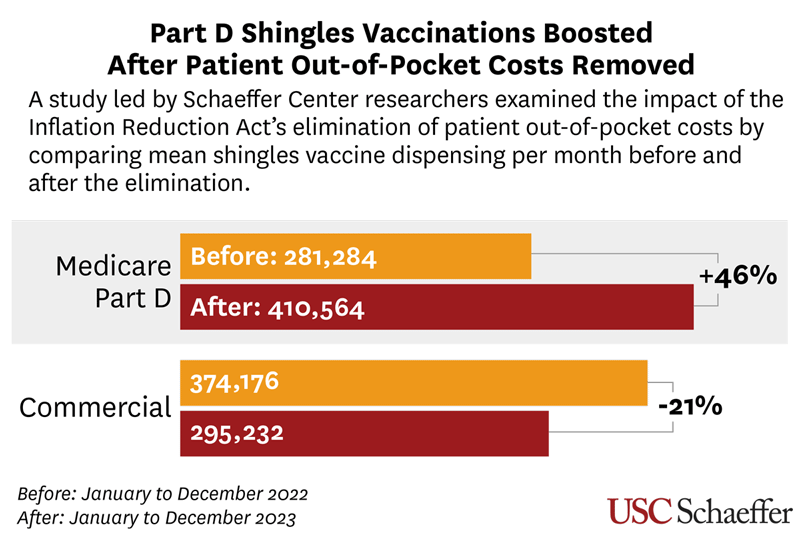
Published as a research letter in JAMA: The Journal of the American Medical Association, the study found that compared to the one year before the implementation of the IRA policy on January 2023, shingles vaccinations covered by Part D rose by 46%.
Physicians recommend the shingles vaccine for adults 50 years and older, since the risk of the viral infection rises with age. Shingles, which affects about one in three people nationally, begins with a painful rash and may lead to the chronic nerve pain of postherpetic neuralgia.
Comparing Part D to commercial insurance, Qato and colleagues found that shingles vaccinations of people with private coverage dropped by 21% over the period examined—from 374,176 per month to 295,231.
“Policy matters,” says Qato, who also directs the Mann School’s Program on Medicines and Public Health and is a senior fellow at the USC Schaeffer Center for Health Policy & Economics. “And when these policies eliminate the costs, they remove barriers in accessing essential medications and preventive services, including vaccinations.”
The research used monthly data from shingles vaccines at retail pharmacies—where 80% of them are administered—between January 2022 and December 2023. However, the researchers emphasize, more research is needed to see if the IRA is making a difference in mitigating disparities in vaccination rates.
“There are more pharmacies located in—and offering—vaccinations in higher-income, white neighborhoods than in communities of color,” Qato observes. “So it’s important to evaluate the impact of policies like the IRA on equity and to ensure that the elimination of cost-sharing reduces—and does not worsen—disparities in shingles vaccination rates.”
“These findings add to the robust evidence base that lowering patient out-of-pocket costs increases the uptake of high-value clinical services,” adds study co-author A. Mark Fendrick, professor of internal medicine and public health at the University of Michigan. “Similar research has demonstrated that similar policies that remove financial barriers, such as those in the IRA, increase access, enhance equity, and ultimately improve health.”
USC Mann Associate Professor John A. Romley, a Schaeffer Center senior fellow, and Rebecca Myerson, a Schaeffer Center nonresident senior fellow, served as co-authors of the study. Dana Goldman—dean and C. Erwin and Ione L. Piper Chair of the USC Price School and co-director of the Schaeffer Center—was also a co-author. The Schaeffer Center is a partnership between the Mann School and the Price School.


